Jade Tomes, Senior medicines optimisation pharmacy technician, Medicines Management Team, Brighton and Hove Clinical Commissioning Group, Part of the Central Sussex and East Surrey Commissioning Alliance, Hove;
Valerie Dowley, Queen’s Nurse and clinical nurse specialist tissue viability, Sussex Community NHS Foundation Trust, Brighton General Hospital, Brighton
Valerie Dowley, Queen’s Nurse and clinical nurse specialist tissue viability, Sussex Community NHS Foundation Trust, Brighton General Hospital, Brighton
ONPOS has been available for over a decade and is currently used in over 40 trusts throughout the UK. It was implemented in Brighton and Hove CCG in the first quarter of 2014. Its use resulted in reduced dressing wastage, instantly accessible dressing stock, improved formulary compliance and more appropriate use of dressings. The real-time data provided by ONPOS also allowed tracking of product use and spend which was then used to inform decision-making and promote a cost-effective culture within the organisation. Since its introduction in 2014, the use of ONPOS has resulted in a 10% decrease in spend, and improved efficiency across primary and community care.
Key points:
Online non-prescription ordering service (ONPOS) | CCG | Wound dressings | Cost savings | Improved efficiencyThe Five Year Forward View (NHS England, 2014) initiated a shift of care delivery into the community, giving clinical commissioning groups (CCGs) responsibility for meeting the needs of an increasingly complex and growing patient population (Guest et al, 2017). CCGs are clinically-led statutory NHS bodies responsible for the planning and commissioning of most secondary care and some primary care/GP services locally, including wound care (Guest et al, 2017).
In 2012/13, 2.2 million wounds were managed by the NHS at an estimated cost of £4.5–5.1 billion, equal to that of obesity. Two thirds of this cost were incurred in the community, and included 18.6 million practice nurse visits, 10.9 million community nurse visits, 7.7 million GP visits, 3.4 million hospital outpatient visits, 97.1 million drug prescriptions and 262.2 million dressings (Guest et al, 2015).
Further analysis revealed that the average CCG with a catchment population of 250,000 adults managed 11,200 wounds in 2012/13, rising to 15,300 wounds in 2015/16. This equates to the prevalence of wounds growing by 11% annually (Figure 1; Guest et al, 2017).
While wound prevalence increases, however, the community nursing workforce is in decline. In the UK, the number of district nurses decreased by 39% between 2002 and 2012, as a result of funding constraints, an increase in the number of nurses leaving practice, increasing rates of retirement and reducing rates of newly qualified nurses (Royal College of Nursing [RCN], 2013).
In 2012/13, 2.2 million wounds were managed by the NHS at an estimated cost of £4.5–5.1 billion, equal to that of obesity. Two thirds of this cost were incurred in the community, and included 18.6 million practice nurse visits, 10.9 million community nurse visits, 7.7 million GP visits, 3.4 million hospital outpatient visits, 97.1 million drug prescriptions and 262.2 million dressings (Guest et al, 2015).
Further analysis revealed that the average CCG with a catchment population of 250,000 adults managed 11,200 wounds in 2012/13, rising to 15,300 wounds in 2015/16. This equates to the prevalence of wounds growing by 11% annually (Figure 1; Guest et al, 2017).
While wound prevalence increases, however, the community nursing workforce is in decline. In the UK, the number of district nurses decreased by 39% between 2002 and 2012, as a result of funding constraints, an increase in the number of nurses leaving practice, increasing rates of retirement and reducing rates of newly qualified nurses (Royal College of Nursing [RCN], 2013).
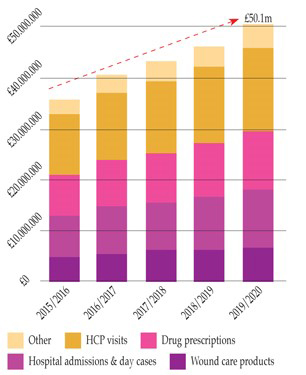
Figure 1. Breakdown in spend and predicted growth of wound care costs at 11% year on year (Guest et al, 2017).
Currently, wound care is managed by a range of healthcare professionals with varying levels of expertise. This, in addition to the number of products available, cost-control measures, and limited evidence for treatment choices has led to fragmented practice and services across the UK, making it unlikely that all patients with wounds have access to good value healthcare (Porter, 2010).
This clearly identifies the need for clinically and cost-effective care delivery if increasing demand and reduced funding are to be balanced without reducing the quality of care provided (Markey and Barrett, 2017; Gray et al, 2018).
In some cases, large improvements in the value of healthcare can be made easily by smarter procurement of services and products (Alderwick et al, 2015) and the implementation of evidence-based guidelines (Ubbink et al, 2014).
In some cases, large improvements in the value of healthcare can be made easily by smarter procurement of services and products (Alderwick et al, 2015) and the implementation of evidence-based guidelines (Ubbink et al, 2014).
ONPOS
ONPOS, an online non-prescription ordering service for wound management dressings, has been available from Coloplast for more than a decade and is currently used by over 40 trusts in the UK, processing over 300 orders per day (Grothier, 2013). Using the service means that dressings can be ordered from an agreed formulary without the need for a prescription. As part of their commitment to partnership working, Coloplast provides ONPOS software installation and training support.The use of ONPOS has been shown in several trusts to provide a number of benefits to improve the efficiency of wound dressing delivery in the community, namely:
- Savings against projected growth; North Tyneside CCG reported a total saving of 22% against projected growth within 6 months of implementation (Milne, 2018)
- Reduction in avoidable product wastage (Grothier, 2011; Griffin, 2015; Markey and Barrett, 2017; Milne, 2018)
- An increased awareness of the cost of dressings among frontline staff (Imburski, 2013; Markey and Barrett, 2017)
- Increased formulary compliance ranging from >85% to 99% post-ONPOS implementation (Knight, 2010; Grothier, 2011; Griffin, 2015; Markey and Barrett, 2017)
- Reduction in time prescribing, and chasing prescriptions (Griffin, 2015; Markey and Barrett, 2017; Milne, 2018)
- Improved monitoring of service and spend as a result of access to real-time data, identifying areas for cost savings and improved efficiency (Grothier, 2013; Griffin, 2015; Markey and Barrett, 2017)
- Improved patient experience (Griffin, 2015; Markey and Barrett, 2017)
- Promotion of joint working resulting in continuity of care (Grothier, 2013; Griffin, 2015; Markey and Barrett, 2017; Milne, 2018)
- Provision of complimentary educational resources and training via the ONPOS portal.
BRIGHTON AND HOVE CCG
Brighton and Hove CCG, part of Central Sussex and East Surrey Commissioning Alliance, provides a range of services to a population of approximately 285,000. This number rises to an estimated 300,000 during the summer months.
The Sussex Community NHS Foundation Trust is a provider for the CCG delivering community health and care services in Brighton and Hove. The CCG area covers 11 community nursing teams, 36 GP surgeries and 26 nursing homes.
The tissue viability service provides specialist advice, support, education and training to frontline staff caring for wounds in Brighton and Hove, with the tissue viability nurse specialist having organisational responsibility for ensuring that care delivery is evidence-based and that limited resources are used to deliver clinically and cost effective care, without adversely impacting quality.
The Sussex Community NHS Foundation Trust is a provider for the CCG delivering community health and care services in Brighton and Hove. The CCG area covers 11 community nursing teams, 36 GP surgeries and 26 nursing homes.
The tissue viability service provides specialist advice, support, education and training to frontline staff caring for wounds in Brighton and Hove, with the tissue viability nurse specialist having organisational responsibility for ensuring that care delivery is evidence-based and that limited resources are used to deliver clinically and cost effective care, without adversely impacting quality.
A steady increase in demand for wound management services and the associated increase in product expenditure has been reported by community health services across the nation (National Prescription Centre, 2012; Guest et al, 2015; 2017). This was also experienced at Brighton and Hove CCG. Furthermore, a number of problems reported by other trusts in the literature were also experienced at Brighton and Hove, including delays in the patient receiving the right product in a timely manner due to delays in the prescribing and dispensing process. As a consequence, clinicians began to over order dressings, to ensure product was available when needed, leading to a large amount of stock wastage.
In order to quantify these problems and inform a service redesign of the way wound care products were procured, a questionnaire was sent to the community nurses which provide the majority of wound care within the trust (n=20). Responses to the questionnaire identified that:
- Most dressing prescriptions were undertaken by GPs
- With access to a wide variety of dressings, formulary compliance, spend and best practice can become difficult to control (Knight, 2010). It was identified in Brighton and Hove, for example, that dressings which appeared first in the drug list on the GP clinical system were frequently prescribed despite not always being the most appropriate choice for the wound. This finding indicated that compliance with the wound product formulary was not being adhered to and incorrect/inappropriate prescribing of product was potentially occurring in some cases
- On average it took longer than one week to supply the patient with the prescribed wound dressing
- Delay in product dispensing was largely down to delays in prescription signing and faxing to pharmacies
- In Brighton and Hove, dressings were ordered through a process in which the community nurse made a request to a GP or a nurse prescriber who then issued a FP10 prescription for the product(s). The local community pharmacist then dispensed the product. This process was proving to be lengthy, with the patient having to wait an unreasonable period of time to access the correct dressing, resulting in delayed implementation of treatment pathways and delayed healing
- Over 50% of the respondents (n=13) spent >30 minutes chasing dressings each week – equivalent to 6.5 hours/week lost to non-clinical work
- Of the respondents, 90% witnessed dressing waste, largely down to changing wound characteristics.
These findings were consistent with those reported elsewhere. Barrett and Markey (2017) reported that a survey carried out at Harrogate and District NHS Trust revealed that 92% of nurses spent one hour each day writing, collecting and organising prescriptions, with 83% of nurses waiting over 10 days to receive prescriptions on some occasions. Following a questionnaire carried out by North Tyneside CCG before the implementation of ONPOS and 6 months after implementation, Milne (2018) reported that pre-ONPOS, 22% of nurses spent over one hour each day chasing prescriptions, falling to only 4% post-implementation.
It is widely recognised that prescribed dressings, once dispensed, become the legal property of the patient, so dressings that are no longer appropriate for the wound characteristics or that are in excess due to pack size exceeding need cannot be used to manage other patients’ wounds (Dimond, 2011).
One audit of a community practice in the West Midlands revealed that 35% of prescribed products remained unused (NPC, 2012). A similar percentage was observed in Brighton and Hove’s FP10 system, resulting in large quantities of prescribed dressings being wasted.
One audit of a community practice in the West Midlands revealed that 35% of prescribed products remained unused (NPC, 2012). A similar percentage was observed in Brighton and Hove’s FP10 system, resulting in large quantities of prescribed dressings being wasted.
However, when considering a non-prescription system for dressing supply, it is important to take into account additional expenditure when considering a change. This includes VAT payment which is not applicable to FP10 items (NPC, 2012).
Based on the findings of the questionnaire, the CCG considered the benefits of using ONPOS and decided to implement the system city wide. The main aim was to improve dressing access, speed up supply and thereby improve treatment pathways, enhance patient care and reduce avoidable waste of products.
Based on the findings of the questionnaire, the CCG considered the benefits of using ONPOS and decided to implement the system city wide. The main aim was to improve dressing access, speed up supply and thereby improve treatment pathways, enhance patient care and reduce avoidable waste of products.
IMPLEMENTATION
ONPOS was implemented over the first quarter of 2014. A decision was taken to start the first wave of change within the 26 nursing homes in January, followed by the community nursing teams and GP surgeries in April 2014. Coloplast worked closely with the CCG Medicines Management Team and the Tissue Viability Service to design flow charts to help staff make a smooth transition. Product stock lists were created to reduce the risk of bulk stocking, and each area was given help to prepare and arrange their product store. This was followed by onsite training of the ONPOS system, issuing of log in details, integrating training in educational sessions and follow-up. Coloplast continued to offer on the ground support over the first year of implementation to ensure everything was running smoothly and liaised very closely with the CCG and tissue viability team when any concerns or queries arose.
Initially, the change from the prescription system to ONPOS was met with resistance from some clinicians for a number of reasons. First, the community nursing teams were concerned that the new system would be more time-consuming and would increase work pressures.
Initially, the change from the prescription system to ONPOS was met with resistance from some clinicians for a number of reasons. First, the community nursing teams were concerned that the new system would be more time-consuming and would increase work pressures.
They had to adapt from dressings being delivered directly to the patient to a system that put the emphasis on the clinician to ensure that appropriate amounts of stock was prepared in advance, bagged and taken to each patient visit.
The community teams had to decide who was responsible for daily stock checks, undertaking twice weekly on-line ordering and the unboxing of large quantities of products delivered to store rooms. It took a number of months to imbed the new way of working and stock management remains an ongoing issue for some teams.
It was also felt that the introduction of the on-line system would result in deskilling of staff in the area of prescribing but in fact it helped to free up valuable time in the long run. By assuring staff that FP10 prescribing of products off formulary was still permitted under special circumstances and in consultation with the TVNS, these fears were allayed.
The community teams had to decide who was responsible for daily stock checks, undertaking twice weekly on-line ordering and the unboxing of large quantities of products delivered to store rooms. It took a number of months to imbed the new way of working and stock management remains an ongoing issue for some teams.
It was also felt that the introduction of the on-line system would result in deskilling of staff in the area of prescribing but in fact it helped to free up valuable time in the long run. By assuring staff that FP10 prescribing of products off formulary was still permitted under special circumstances and in consultation with the TVNS, these fears were allayed.
ONPOS BENEFITS
Product waste reduction
As expected, the use of ONPOS resulted in a more efficient ordering system, better management of first-line stock and therefore less product waste. Previously, the prescribed dressings became the property of the patient once dispensed and delivered to them whereas dressings purchased via ONPOS remained the property of the CCG. This new system allowed the storage of products in community nursing hubs, stock cupboards in nursing homes and GP surgeries where products could be readily accessed, boxes of products split and used as needed, thereby minimizing waste. Clinicians, tissue viability and Coloplast decided on maximum and minimum stock storage levels and created labels and product stock-taking sheets to help maintain suitable stock levels.Some trusts, where ONPOS has been successfully implemented, report a reduction or elimination of ‘boot or grey stock’. This term is used to describe the illegal practice in which dressings that are no longer needed by the patient but are legally owned by them (as are prescribed for them individually)are often carried by nurses in the boot of their cars, to be used on other patients (Grothier, 2011; Griffin, 2013). In Brighton and Hove post-ONPOS, spare stock is still carried in the boot of cars as clinicians are still finding that due to work pressures, essential stock is not being bagged ready for patients in a timely manner. However, as this stock is owned by the CCG rather than the patient, this is no longer a legal issue.
Before the implementation of ONPOS, patients attending leg ulcer clinics would need to bring their prescribed dressings and compression bandaging along to clinic appointments. If the patient was unable to carry it, forgot to bring it or if the dressing was no longer appropriate
due to a change in wound condition, this led to ‘making do’ with the
products available to bridge the gap until a new prescription could be issued. Post-ONPOS a range of stock was instantly accessible, allowing for immediate selection of the most suitable product(s).
Immediate dressing availability via ONPOS also resulted in a reduction of ‘just in case’ ordering of extra dressings on FP10. Now now patients can access the right dressing at the right time across all care settings.
Awareness of product cost
A surprising outcome of the implementation of ONPOS was that it allowed the clinicians who undertake the online ordering to see the cost of dressing stock. This has resulted in them becoming more mindful of ensuring that ordering and usage is appropriate and cost effective where possible.Increased formulary compliance and control
The use of ONPOS had a positive impact on formulary compliance improving it to 95%, in line with findings from several other trusts in the UK (Knight, 2010; Grothier, 2013; Griffin, 2015; Markey and Barrett, 2017). During the implementation it was agreed that advanced wound dressings or very costly products would require tissue viability approval before going to the pharmacy for dispensing. This has resulted in the tissue viability service gaining better oversight of what is being ordered, the amount of advanced wound dressings being prescribed and the justification for these decisions.Improved patient experience
The use of ONPOS improved patient experience by enabling access to the most appropriate dressing as soon as possible, leading to better patient experience. It allowed clinicians to put in place timely treatment changes, based on clinical wound assessment findings by altering the dressing regimen if and when required. There were no longer any prescribing issues or dispensing delays to navigate.Using ONPOS also had a positive impact on GP and practice nurse time as they were no longer required to generate and sign routine prescriptions. The time could then be freed up for direct patient contact. An incidental cost improvement was also noted. Often the initial GP prescription was generated by the GP’s admin team who had limited knowledge of the products that clinicians were asking for, and therefore often selected wound products by alphabetical order. This resulted in antimicrobial silver (Ag) products being prescribed, at more expense than non-antimicrobial dressings, simply because the ‘Ag’ came up first on the product list on their electronic system.
Real-time data
The monthly reports produced by ONPOS enabled the CCG and Trust to have a very clear view of dressing spend and use across one or more locations by gathering and analyzing information. Monthly face to face meetings between Brighton and Hove and Coloplast representatives to review the ONPOS dashboard allowed the tissue viability service to identify areas of high/inappropriate spend issues and to ascertain whether there were training needs to meet the specific issues of individual areas. The real-time data of spend, location and products used also enabled realistic budgeting and the negotiation of costs with suppliers. It allowed the implementation of strategies to work smarter.The access to live data and ability to respond to the findings realized instant savings when changing products to more cost-effective alternatives, with no adverse effect on clinical outcomes. For example, the data provided in one report enabled identification of the high usage of antimicrobial dressings.
However, ONPOS data relating to dressing spend is collected on a separate system to other prescribed items, e.g. hosiery, so the information needs to be analysed separately or collated within the Trust.
Cost savings
The use of ONPOS has resulted in significant cost savings year on year since its implementation in 2014 to February 2018 (Figure 2). These savings are inclusive of VAT costs incurred when using a non-prescription system and are a result of improved formulary adherence, the monitoring of specific, prescribed specialist dressing items, reduction of waste, access to real-time data to inform decision-making and training and promotion of a cost-aware culture (Figure 3).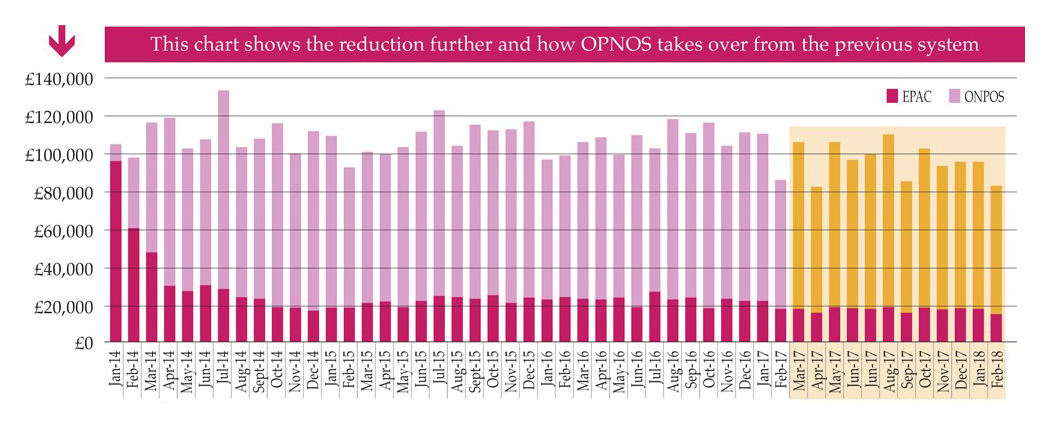
Figure 2. Year on year savings gained by use of ONPOS compared to previously used system
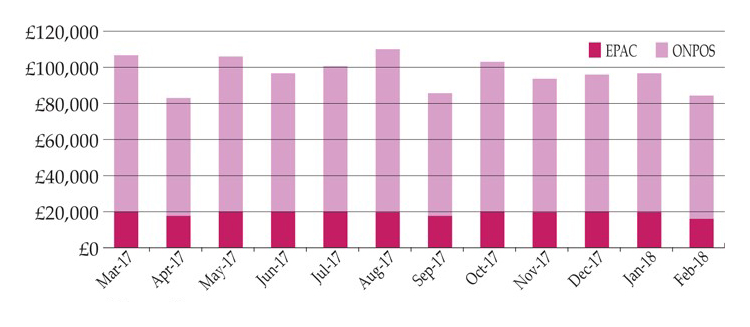
Figure 3. Savings gained by use of ONPOS compared to previously used system
Educational support
ONPOS can be used with ‘non-ordering access’, enabling staff to access educational materials, including local policies and guidelines as well as national guidelines and a library of wound literature as part of Coloplast’s Healthcare Excellence through Access and Learning (HEAL) educational initiative. The availability of a platform for staff to access educational materials in conjunction with ONPOS mean that not only is efficiency improved but education and training based on best practice recommendations underpins practice. In addition, Coloplast produce an award-winning range of wound care products that can be used as part of wound care delivery.CONCLUSIONS
ONPOS enables formulary wound dressing products to be purchased from a chosen supply route (e.g. supply chain, local pharmacy or wholesalers) without needing a prescription or paperwork.
Brighton and Hove CCG adopted ONPOS after identifying a number of problems with wound dressing supply. Inefficient prescribing of dressings and product wastage have previously been identified as two major barriers to the delivery of an efficient wound care service in a community setting
(Knight, 2010; Grothier, 2013; North of England NHS Commercial Procurement Collaborative, 2013; Griffin, 2015).
The use of the ONPOS system enabled clinicians faster access to wound dressings. The ability to monitor dressing usage in real time enabled greater visibility of product use, supply and control. In turn, inefficiencies or gaps in wound care dressing provision were identified and improved.
Brighton and Hove CCG adopted ONPOS after identifying a number of problems with wound dressing supply. Inefficient prescribing of dressings and product wastage have previously been identified as two major barriers to the delivery of an efficient wound care service in a community setting
(Knight, 2010; Grothier, 2013; North of England NHS Commercial Procurement Collaborative, 2013; Griffin, 2015).
The use of the ONPOS system enabled clinicians faster access to wound dressings. The ability to monitor dressing usage in real time enabled greater visibility of product use, supply and control. In turn, inefficiencies or gaps in wound care dressing provision were identified and improved.
Likewise, good practice was noted and shared. The sharing of this information created accountability and fostered a cost-aware culture among front-line staff, improving formulary compliance to 95%.
The adoption of ONPOS by Brighton and Hove CCG has resulted in a 10% decrease in dressing spend through smarter procurement of product at a time when costs are predicted to grow by 11% year on year (Guest et al, 2017). The use of ONPOS has also led to improved efficiency to the benefit of both the patient and healthcare provider services, against a backdrop of increasing service demand, and reduced budget and resource.
The writing of this article was supported by an educational grant from Coloplast Ltd.
The adoption of ONPOS by Brighton and Hove CCG has resulted in a 10% decrease in dressing spend through smarter procurement of product at a time when costs are predicted to grow by 11% year on year (Guest et al, 2017). The use of ONPOS has also led to improved efficiency to the benefit of both the patient and healthcare provider services, against a backdrop of increasing service demand, and reduced budget and resource.
The writing of this article was supported by an educational grant from Coloplast Ltd.
References
Alderwick H, Robertson R, Appleby J, et al (2015) Better value in the NHS: the role of changes in clinical practice. The King’s Fund, London
Barrett S, Markey P (2017) The benefit of using an online ordering service to improve efficiency in wound care services. Br J Health Care Management 23(11): 517–23
Dimond B (2011) Legal Aspects of Nursing. Pearson Education, Harlow
Gray TA, Rhodes S, Atkinson RA, et al (2018) Opportunities for better value wound care: a multiservice, cross-sectional survey of complex wounds and their care in the UK community population. Br Med J Open Access
Griffin J (2015) Driving efficiencies in wound care expenditure through service redesign utilizing an online non-prescription ordering service. Wounds UK 11(3): 1–6
Griffin J (2013) Reviewing the impact of online non-prescription supply of wound care dressings — ONPOS. Poster presentation, Wounds UK, Harrogate
Grothier L (2011) Using ONPOS to implement the QIPP Agenda. Poster presentation, Wound UK, Harrogate
Grothier L (2013) Reflections on the implementation of a web-based non-prescription ordering system. Wounds UK 9(2): 51–5
Guest JF, Ayoub N, McIlwraith T, et al (2015) Health economic burden that wounds impose on the National Health Service in the UK. BMJ Open 5: e009283. doi:10.1136/bmjopen-2015-009283. Available online: http://bmjopen.bmj.com/content/5/12/e009283
Guest JF, Vowden K, Vowden P (2017) The health economic burden that acute and chronic wounds impose on an average clinical commissioning group/health board in the UK. J Wound Care 26(6): 292–303
Humber NHS Foundation Trust (2013) NOE CPC Case Study. Wound Care dressings community distribution service. North of England NHS Commercial Procurement Collaborative, Humber NHS Foundation Trust
Imbirski K (2013) Utilising ONPOS to change practice and reduce waste within an integrated care team. Poster presentation, Wounds UK, Harrogate
Knight S (2010) Introducing a new method of providing wound care products. Wounds UK 6(2): 66–73
Markey P, Barrett S (2017) The benefits of using an online ordering service to improve efficiency in wound care services. Br J Healthcare Manage 23(11): 1–7
Milne J (2018) Comparison of survey results prior to and 6 months following the introduction of an online non-prescription ordering service. Poster. Wound Care Today, Milton Keynes, June 2018
NHS England (2014) Five Year Forward View. NHS England, London. Available online: www.england.nhs.uk/wp- content/uploads/2014/10/5yfv-web.pdf
North of England NHS Commercial Procurement Collaborative (2013) Wound care dressings community distribution service. North of England NHS Commercial Procurement Collaborative, Humber NHS Foundation Trust
National Prescription Centre (2012) Key Therapeutics Topics – Medicines Management Options for Local Implementation. NICE, London
Porter ME (2010) What is value in health care? N Engl J Med 363: 2477–81
Royal College of Nursing (2013) Frontline First: Nursing on Red Alert April 2013. RCN. London. Available online: https://my.rcn.org.uk/__data/assets/pdf_file/0003/518376/004446.pdf
(accessed 19/09/2017)
Ubbink DT, Santema TB, Stoekenbroek RM (2014) Systemic wound care: a meta-review of Cochrane systematic reviews. Surg Technol Int 24: 99–111
Barrett S, Markey P (2017) The benefit of using an online ordering service to improve efficiency in wound care services. Br J Health Care Management 23(11): 517–23
Dimond B (2011) Legal Aspects of Nursing. Pearson Education, Harlow
Gray TA, Rhodes S, Atkinson RA, et al (2018) Opportunities for better value wound care: a multiservice, cross-sectional survey of complex wounds and their care in the UK community population. Br Med J Open Access
Griffin J (2015) Driving efficiencies in wound care expenditure through service redesign utilizing an online non-prescription ordering service. Wounds UK 11(3): 1–6
Griffin J (2013) Reviewing the impact of online non-prescription supply of wound care dressings — ONPOS. Poster presentation, Wounds UK, Harrogate
Grothier L (2011) Using ONPOS to implement the QIPP Agenda. Poster presentation, Wound UK, Harrogate
Grothier L (2013) Reflections on the implementation of a web-based non-prescription ordering system. Wounds UK 9(2): 51–5
Guest JF, Ayoub N, McIlwraith T, et al (2015) Health economic burden that wounds impose on the National Health Service in the UK. BMJ Open 5: e009283. doi:10.1136/bmjopen-2015-009283. Available online: http://bmjopen.bmj.com/content/5/12/e009283
Guest JF, Vowden K, Vowden P (2017) The health economic burden that acute and chronic wounds impose on an average clinical commissioning group/health board in the UK. J Wound Care 26(6): 292–303
Humber NHS Foundation Trust (2013) NOE CPC Case Study. Wound Care dressings community distribution service. North of England NHS Commercial Procurement Collaborative, Humber NHS Foundation Trust
Imbirski K (2013) Utilising ONPOS to change practice and reduce waste within an integrated care team. Poster presentation, Wounds UK, Harrogate
Knight S (2010) Introducing a new method of providing wound care products. Wounds UK 6(2): 66–73
Markey P, Barrett S (2017) The benefits of using an online ordering service to improve efficiency in wound care services. Br J Healthcare Manage 23(11): 1–7
Milne J (2018) Comparison of survey results prior to and 6 months following the introduction of an online non-prescription ordering service. Poster. Wound Care Today, Milton Keynes, June 2018
NHS England (2014) Five Year Forward View. NHS England, London. Available online: www.england.nhs.uk/wp- content/uploads/2014/10/5yfv-web.pdf
North of England NHS Commercial Procurement Collaborative (2013) Wound care dressings community distribution service. North of England NHS Commercial Procurement Collaborative, Humber NHS Foundation Trust
National Prescription Centre (2012) Key Therapeutics Topics – Medicines Management Options for Local Implementation. NICE, London
Porter ME (2010) What is value in health care? N Engl J Med 363: 2477–81
Royal College of Nursing (2013) Frontline First: Nursing on Red Alert April 2013. RCN. London. Available online: https://my.rcn.org.uk/__data/assets/pdf_file/0003/518376/004446.pdf
(accessed 19/09/2017)
Ubbink DT, Santema TB, Stoekenbroek RM (2014) Systemic wound care: a meta-review of Cochrane systematic reviews. Surg Technol Int 24: 99–111


