References
Abouhamda A, Alturkstani M, Jan Y (2019) Lower sensitivity of ankle-brachial index measurements among people suffering with diabetes-associated vascular disorders: A systematic review. SAGE open medicine 7, 2050312119835038
Alavi A, Sibbald RG, Nabavizadeh R, Valaei F, Coutts P, Mayer D (2015) Audible handheld Doppler ultrasound determines reliable and inexpensive exclusion of significant peripheral arterial disease. Vascular 23(6): 622–9
British Lymphology Society (2018) Position Paper for Ankle Brachial Pressure Index (ABPI). Informing decision making prior to the application of compression therapy. Available online: www.thebls.com
Brownrigg JRW, Schaper NC, Hinchcliffe RJ (2015) Diagnosis and assessment of peripheral arterial disease in the diabetic foot. Diabetic Med 32(6): 738–47
Buerger L (1924) Circulatory disturbances of the extremities. WB Saunders, Philadelphia: 162–8
Charnogursky G, Lee H, Lopez N (2014) Diabetic neuropathy. In: Handbook of Clinical Neurology. Vol 120. Elsevier: 773–85
Clayton W, Elsay TA (2009) A review of the pathophysiology, classification, and treatment of foot ulcers in diabetic patients. Clin Diabetes 27(2): 52–8
Concannon MJ, Sharpe A (2012) The importance of screening for Charcot neuroarthropathy. Practice Nurs 23(8), published online 29 Sept 2013
Conte MS, Bradbury AW, Kolh P, White JV, Dick F, Fitridge R, et al (2019) Global vascular guidelines on the management of chronic limb-threatening ischemia. J Vasc Surg 69(6S): 3S–125S
Department of Health (2019) The 9th annual report from the Advisory Committee on Antimicrobial Prescribing, Resistance and Healthcare Associated Infection (APRHAI). APRHAI annual report, 2017 to 2018. Available online: www.gov.uk/government/publications/aprhai-annual-report-2017-to-2018 (accessed 19 January, 2020)
Dolan NC, Liu K, Criqui MH, Greenland P, Guralnik JM, Chan C, et al (2002) Peripheral artery disease, diabetes, and reduced lower extremity functioning. Diabetes Care 25(1): 113–20
Guest JF, Fuller GW, Vowden P (2018) Diabetic foot ulcer management in clinical practice in the UK: costs and outcomes. Int Wound J 15(1): 43–52
Hinchliffe RJ, Forsythe RO, Apelqvist J, Boyko EJ, Fitridge R, Pio Hong J, et al on behalf of the International Working Group on the Diabetic Foot (2019) IWGDF Guideline on diagnosis, prognosis and management of peripheral artery disease in patients with a foot ulcer and diabetes. Available online: www.iwgdfguidelines.org
Hingorani A, LaMuraglia GM, Henke P, Meissner MH, Loretz L, Zinszer KM, et al (2016) The management of diabetic foot: A clinical practice guideline by the Society for Vascular Surgery in collaboration with the American Podiatric Medical Association and the Society for Vascular Medicine. J Vasc Surg 63(2 Suppl): 3S–21S
International Wound Infection Institute (2016) Wound Infection in Clinical Practice. International Consensus. Wounds International, London. Available online: https://bit.ly/2iWLDAc (accessed 9 January, 2020)
Jeffcoate WJ, Harding KG (2003) Diabetic foot ulcers. Lancet 361(9368): 1545–51
Keast D, Swanson T, Carville K, Fletcher J, Schultz G, Black J (2014) Ten Top Tips... understanding and managing wound biofilm. Wounds Int 5(2): 20–4
Lend GC, Fowkes FGR (1992) The Edinburgh Claudication Questionnaire: An improved version of the WHO/Rose questionnaire for use in epidemiological surveys. J Clin Epidemiol 45(10): 1101–09
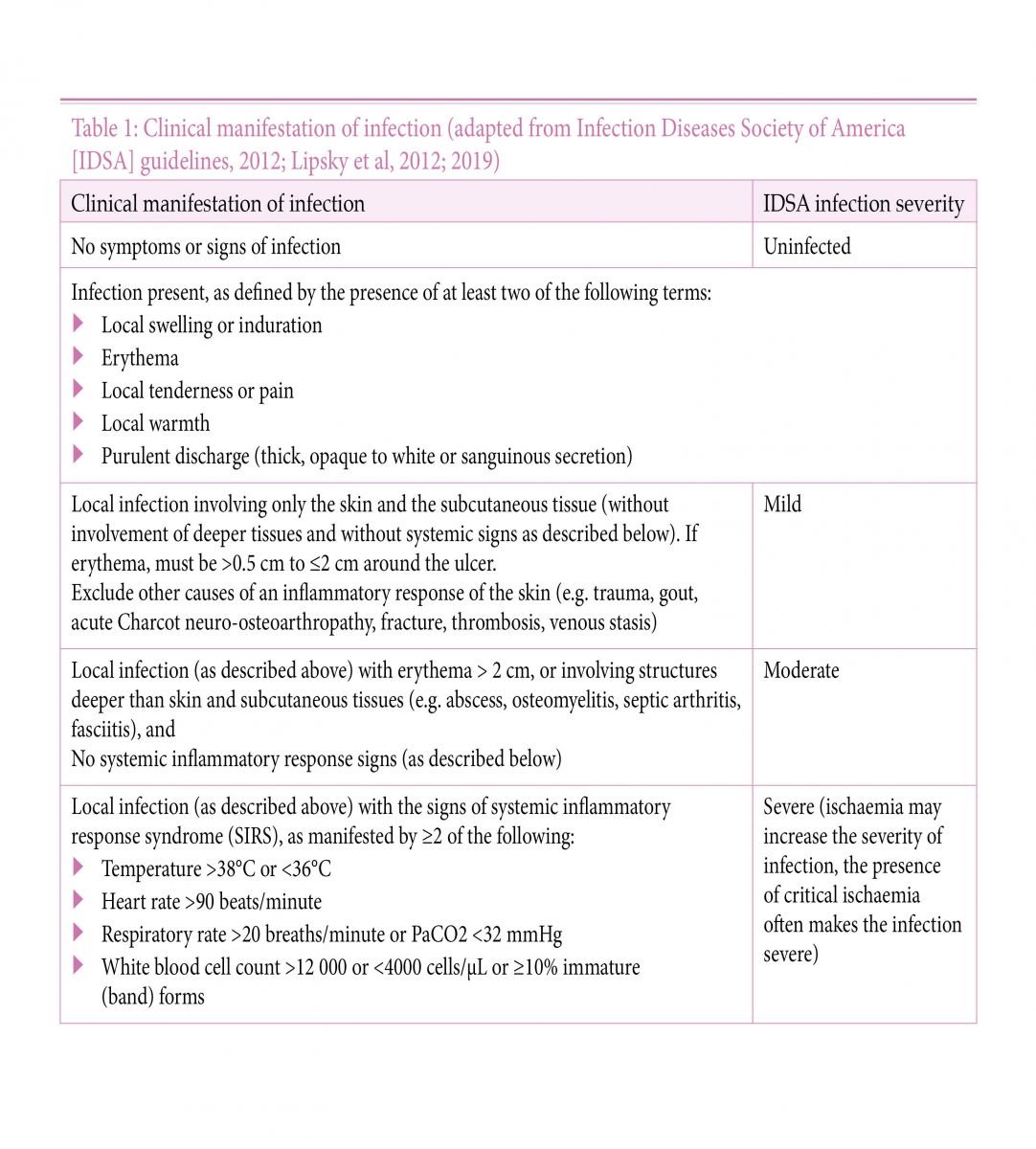
Lipsky BA, Berendt AR, Cornia PB, Pile JC, Peters EJG, Armstrong DG, et al (2012) 2012 Infection Diseases Society of America Clinical Practice Guidelines for the Diagnosis and Treatment of Diabetic Foot Infections. Clin Infect Dis 54(12): e132–2173
Lipsky BA, Senneville E, Abbas ZG, Aragón-Sánchez J, Diggle M, Embiln J, et al on behalf of the International Working Group on the Diabetic Foot (2019) IWGDF Guideline on the diagnosis and treatment of foot infection in persons with diabetes. Available online: www.iwgdfguidelines.org
Lundin M, Wiksten JP, Peräkylä T, Lindfors O, Savolainen H, Skyttä J, et al (1999) Distal pulse palpation: is it reliable? World J Surg 23(3): 252–5
McGee SR, Boyko EJ (1998) Physical examination and chronic lower-extremity ischemia: a critical review. Arch Intern Med 158(12): 1357–64
National Diabetes Footcare Audit (2019) National Diabetes Footcare Audit, 2014–2018. Available online: https://digital.nhs.uk/data-and-information/publications/statistical/national-diabetes-footcare-audit/2014-2018. Accessed 19/01/2020
National Heart, Lung and Blood Institute (2019) Peripheral Arterial Disease. Available online: www.nhlbi.nih.gov/health-topics/peripheral-artery-disease (accessed 9 January, 2020)
National Institute for Health and Care Excellence (2018) Peripheral arterial disease: diagnosis and management. Clinical guideline [CG147]. NICE, London. Available online: www.nice.org.uk/guidance/cg147
National Institute for Health and Care Excellence (2019) Diabetic foot problems: prevention and management. NG19. NICE, London. Available online: www.nice.org.uk/guidance/ng19 (accessed 19 January, 2020)
Pham H, Armstrong DG, Harvey C, et al (2000) Screening techniques to identify people at high risk for diabetic foot ulceration: a prospective multicentre trial. Diabetes Care 23: 606–11
Prompers L, Huijberts M, Apelqvist J, Jude E, Piaggesi A, Bakker K, et al (2007) High prevalence of ischaemia, infection and serious comorbidity in patients with diabetic foot disease in Europe. Baseline results from the Eurodiale study. Diabetlogia 50(1): 18–25
Rogers LC, Frykberg RG, Armstrong DG, Boulton AJM, Edmonds M, Ha Van G, et al (2011) The Charcot foot in diabetes. Diabetes Care 34(9): 2123–29
Scissons R (2008) Characterizing triphasic, biphasic, and monophasic Doppler waveforms: should a simple task be so difficult? J Diagnostic Med Sonography 24(5): 269–76
Society for Vascular Surgery Lower Extremity Guidelines Writing Group, Conte MS, Pomposelli FB, et al (2015) Society for Vascular Surgery practice guidelines for atherosclerotic occlusive disease of the lower extremities: management of asymptomatic disease and claudication. J Vasc Surg 61(3 suppl): 2S–41S
Teo KK (2019) Occlusive Peripheral Arterial Disease. MSD Manual. Available online: www.msdmanuals.com/en-gb/home/heart-and-blood-vessel-disorders/peripheral-arterial-disease/occlusive-peripheral-arterial-disease (accessed 9 January, 2020)
Alavi A, Sibbald RG, Nabavizadeh R, Valaei F, Coutts P, Mayer D (2015) Audible handheld Doppler ultrasound determines reliable and inexpensive exclusion of significant peripheral arterial disease. Vascular 23(6): 622–9
British Lymphology Society (2018) Position Paper for Ankle Brachial Pressure Index (ABPI). Informing decision making prior to the application of compression therapy. Available online: www.thebls.com
Brownrigg JRW, Schaper NC, Hinchcliffe RJ (2015) Diagnosis and assessment of peripheral arterial disease in the diabetic foot. Diabetic Med 32(6): 738–47
Buerger L (1924) Circulatory disturbances of the extremities. WB Saunders, Philadelphia: 162–8
Charnogursky G, Lee H, Lopez N (2014) Diabetic neuropathy. In: Handbook of Clinical Neurology. Vol 120. Elsevier: 773–85
Clayton W, Elsay TA (2009) A review of the pathophysiology, classification, and treatment of foot ulcers in diabetic patients. Clin Diabetes 27(2): 52–8
Concannon MJ, Sharpe A (2012) The importance of screening for Charcot neuroarthropathy. Practice Nurs 23(8), published online 29 Sept 2013
Conte MS, Bradbury AW, Kolh P, White JV, Dick F, Fitridge R, et al (2019) Global vascular guidelines on the management of chronic limb-threatening ischemia. J Vasc Surg 69(6S): 3S–125S
Department of Health (2019) The 9th annual report from the Advisory Committee on Antimicrobial Prescribing, Resistance and Healthcare Associated Infection (APRHAI). APRHAI annual report, 2017 to 2018. Available online: www.gov.uk/government/publications/aprhai-annual-report-2017-to-2018 (accessed 19 January, 2020)
Dolan NC, Liu K, Criqui MH, Greenland P, Guralnik JM, Chan C, et al (2002) Peripheral artery disease, diabetes, and reduced lower extremity functioning. Diabetes Care 25(1): 113–20
Guest JF, Fuller GW, Vowden P (2018) Diabetic foot ulcer management in clinical practice in the UK: costs and outcomes. Int Wound J 15(1): 43–52
Hinchliffe RJ, Forsythe RO, Apelqvist J, Boyko EJ, Fitridge R, Pio Hong J, et al on behalf of the International Working Group on the Diabetic Foot (2019) IWGDF Guideline on diagnosis, prognosis and management of peripheral artery disease in patients with a foot ulcer and diabetes. Available online: www.iwgdfguidelines.org
Hingorani A, LaMuraglia GM, Henke P, Meissner MH, Loretz L, Zinszer KM, et al (2016) The management of diabetic foot: A clinical practice guideline by the Society for Vascular Surgery in collaboration with the American Podiatric Medical Association and the Society for Vascular Medicine. J Vasc Surg 63(2 Suppl): 3S–21S
International Wound Infection Institute (2016) Wound Infection in Clinical Practice. International Consensus. Wounds International, London. Available online: https://bit.ly/2iWLDAc (accessed 9 January, 2020)
Jeffcoate WJ, Harding KG (2003) Diabetic foot ulcers. Lancet 361(9368): 1545–51
Keast D, Swanson T, Carville K, Fletcher J, Schultz G, Black J (2014) Ten Top Tips... understanding and managing wound biofilm. Wounds Int 5(2): 20–4
Lend GC, Fowkes FGR (1992) The Edinburgh Claudication Questionnaire: An improved version of the WHO/Rose questionnaire for use in epidemiological surveys. J Clin Epidemiol 45(10): 1101–09
Lipsky BA, Berendt AR, Cornia PB, Pile JC, Peters EJG, Armstrong DG, et al (2012) 2012 Infection Diseases Society of America Clinical Practice Guidelines for the Diagnosis and Treatment of Diabetic Foot Infections. Clin Infect Dis 54(12): e132–2173
Lipsky BA, Senneville E, Abbas ZG, Aragón-Sánchez J, Diggle M, Embiln J, et al on behalf of the International Working Group on the Diabetic Foot (2019) IWGDF Guideline on the diagnosis and treatment of foot infection in persons with diabetes. Available online: www.iwgdfguidelines.org
Lundin M, Wiksten JP, Peräkylä T, Lindfors O, Savolainen H, Skyttä J, et al (1999) Distal pulse palpation: is it reliable? World J Surg 23(3): 252–5
McGee SR, Boyko EJ (1998) Physical examination and chronic lower-extremity ischemia: a critical review. Arch Intern Med 158(12): 1357–64
National Diabetes Footcare Audit (2019) National Diabetes Footcare Audit, 2014–2018. Available online: https://digital.nhs.uk/data-and-information/publications/statistical/national-diabetes-footcare-audit/2014-2018. Accessed 19/01/2020
National Heart, Lung and Blood Institute (2019) Peripheral Arterial Disease. Available online: www.nhlbi.nih.gov/health-topics/peripheral-artery-disease (accessed 9 January, 2020)
National Institute for Health and Care Excellence (2018) Peripheral arterial disease: diagnosis and management. Clinical guideline [CG147]. NICE, London. Available online: www.nice.org.uk/guidance/cg147
National Institute for Health and Care Excellence (2019) Diabetic foot problems: prevention and management. NG19. NICE, London. Available online: www.nice.org.uk/guidance/ng19 (accessed 19 January, 2020)
Pham H, Armstrong DG, Harvey C, et al (2000) Screening techniques to identify people at high risk for diabetic foot ulceration: a prospective multicentre trial. Diabetes Care 23: 606–11
Prompers L, Huijberts M, Apelqvist J, Jude E, Piaggesi A, Bakker K, et al (2007) High prevalence of ischaemia, infection and serious comorbidity in patients with diabetic foot disease in Europe. Baseline results from the Eurodiale study. Diabetlogia 50(1): 18–25
Rogers LC, Frykberg RG, Armstrong DG, Boulton AJM, Edmonds M, Ha Van G, et al (2011) The Charcot foot in diabetes. Diabetes Care 34(9): 2123–29
Scissons R (2008) Characterizing triphasic, biphasic, and monophasic Doppler waveforms: should a simple task be so difficult? J Diagnostic Med Sonography 24(5): 269–76
Society for Vascular Surgery Lower Extremity Guidelines Writing Group, Conte MS, Pomposelli FB, et al (2015) Society for Vascular Surgery practice guidelines for atherosclerotic occlusive disease of the lower extremities: management of asymptomatic disease and claudication. J Vasc Surg 61(3 suppl): 2S–41S
Teo KK (2019) Occlusive Peripheral Arterial Disease. MSD Manual. Available online: www.msdmanuals.com/en-gb/home/heart-and-blood-vessel-disorders/peripheral-arterial-disease/occlusive-peripheral-arterial-disease (accessed 9 January, 2020)